Prior Authorization
For some types of care, your primary care provider (PCP) or specialist will need to get permission from HPSM before you get care. This is called prior authorization, prior approval or pre-approval. Prior authorization lets HPSM make sure the care is medically necessary. This means it needs to be reasonable and necessary to protect your life, keep you from becoming seriously ill or disabled, or alleviate severe pain.
- For emergency care, including having a baby, you never need prior authorization. Even out-of-network emergency care is covered.
- Some non-emergency services that always require prior authorization.
Check if you need prior authorization
To check if you need prior authorization, either use HPSM’s search tool, download HPSM's Prior Authorization Required List, or ask your PCP.
To use the search tool:
- Enter a keyword, description or five-digit Current Procedural Terminology (CPT®) code into the search field. CPT codes are used for medical billing and claims processing. They are five digits long and can have numbers and letters or only numbers. The American Medical Association (AMA) created CPT codes to ensure that healthcare providers can:
- Uniformly report medical services they performed
- Get paid the right amount for healthcare services performed
- Give members itemized bills listing the exact services they performed
- Choose a service from the drop-down list for information:
- “Results as of” shows the date and time you searched for the information
- “Code” shows the CPT code
- “Description” shows the service description from the list of standardized CPT codes. This search tool includes all CPT codes that require prior authorization
- “PA requirement status (Yes/Conditional)” shows whether a service requires prior authorization.
- If "Yes" or "Conditional" appear in the search results, then the service requires prior authorization. However, that does not mean it is a covered benefit. Prior authorization is based on medical necessity and search results do not guarantee coverage or eligibility. To find out if a service is a covered benefit, you must call your provider or HPSM. If the code you look up appears in the search results, you must ask your provider to complete and submit a Prior Authorizations Request Form. Wait for authorization approval from HPSM before getting the service.
- “Date Updated” shows the last time the American Medical Association (AMA) changed this CPT code. Code lists are updated quarterly.
Only CPT codes that require prior authorization are listed in this PDF. Codes that are not on this list do not require prior authorization. Note that a treatment can have multiple procedure codes. If you do not know the procedure code(s) or name(s) for the treatment you want, ask your provider.
To use the list offline, download and save the PDF to your computer or device.
To get your PCP’s phone number, log in to the Member Portal.
Some services always need prior authorization
The following services always require prior authorization, even if you get them from an HPSM network provider:
- Hospitalization, including long term care
- Services outside of the HPSM service area
- Outpatient surgery
- Long-term therapy
- Specialized care
- Specialized radiology procedures (such as a CT scan or an MRI)
Prior Authorization Code Search Tool
Prior Authorization Code Lists
Medical PAR list
Standard Prior Authorization Requests
Responses to standard (non-urgent) prior authorization are due to providers within seven (7) calendar days. In 2025 we received a total of 8677 standard prior authorization requests for our covered patients. 96.1% of those requests were approved.
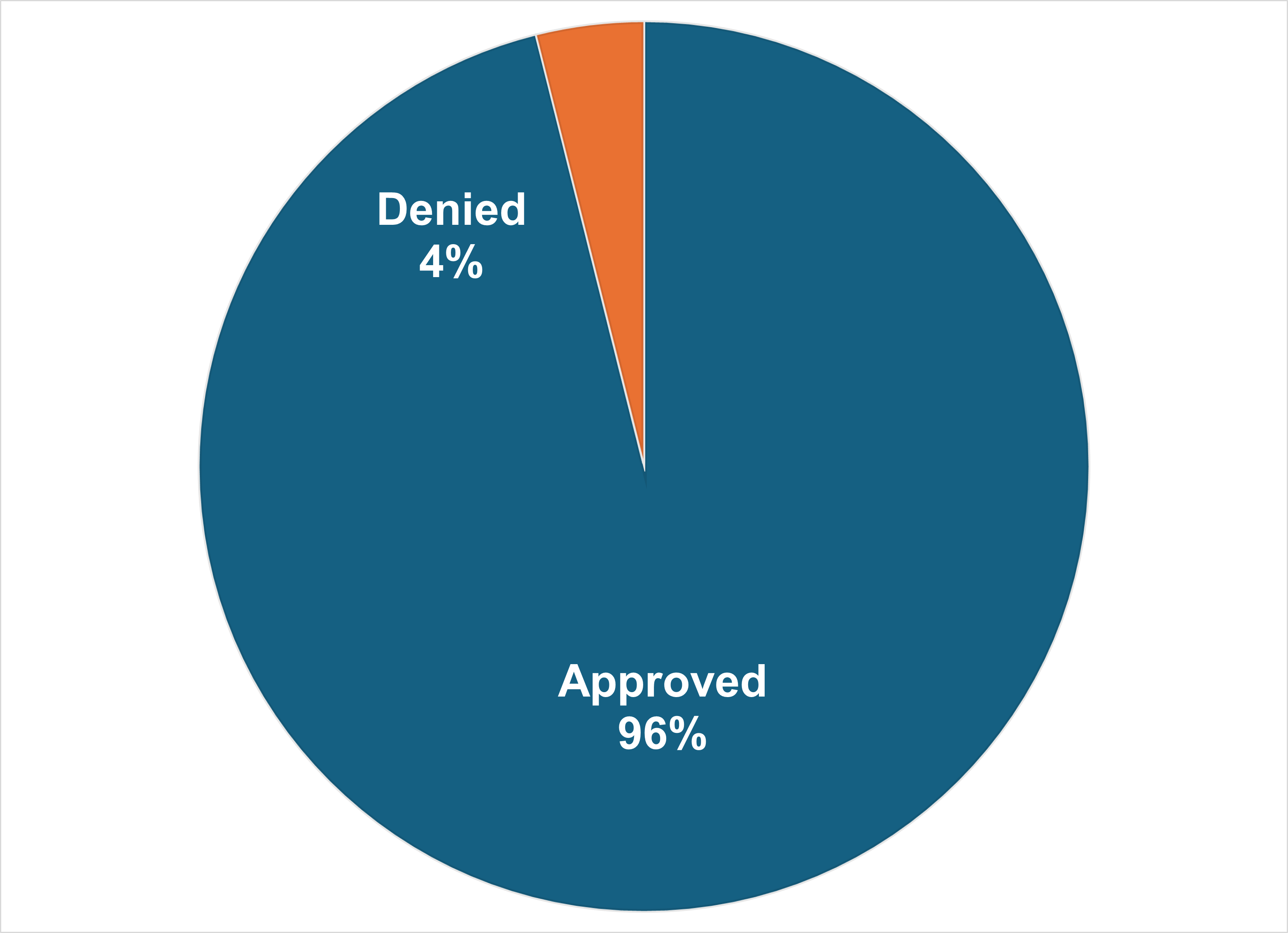
- Mean (average) time to make decisions: 2.8 days
- Median (middle) time to make decision: 2 days
Expedited Prior Authorization Requests
Responses to expedited (urgent) prior authorization are due to providers within three (3) days. In 2025 we received a total of 589 expedited prior authorization requests for our covered patients. 93.7% of those requests were approved.
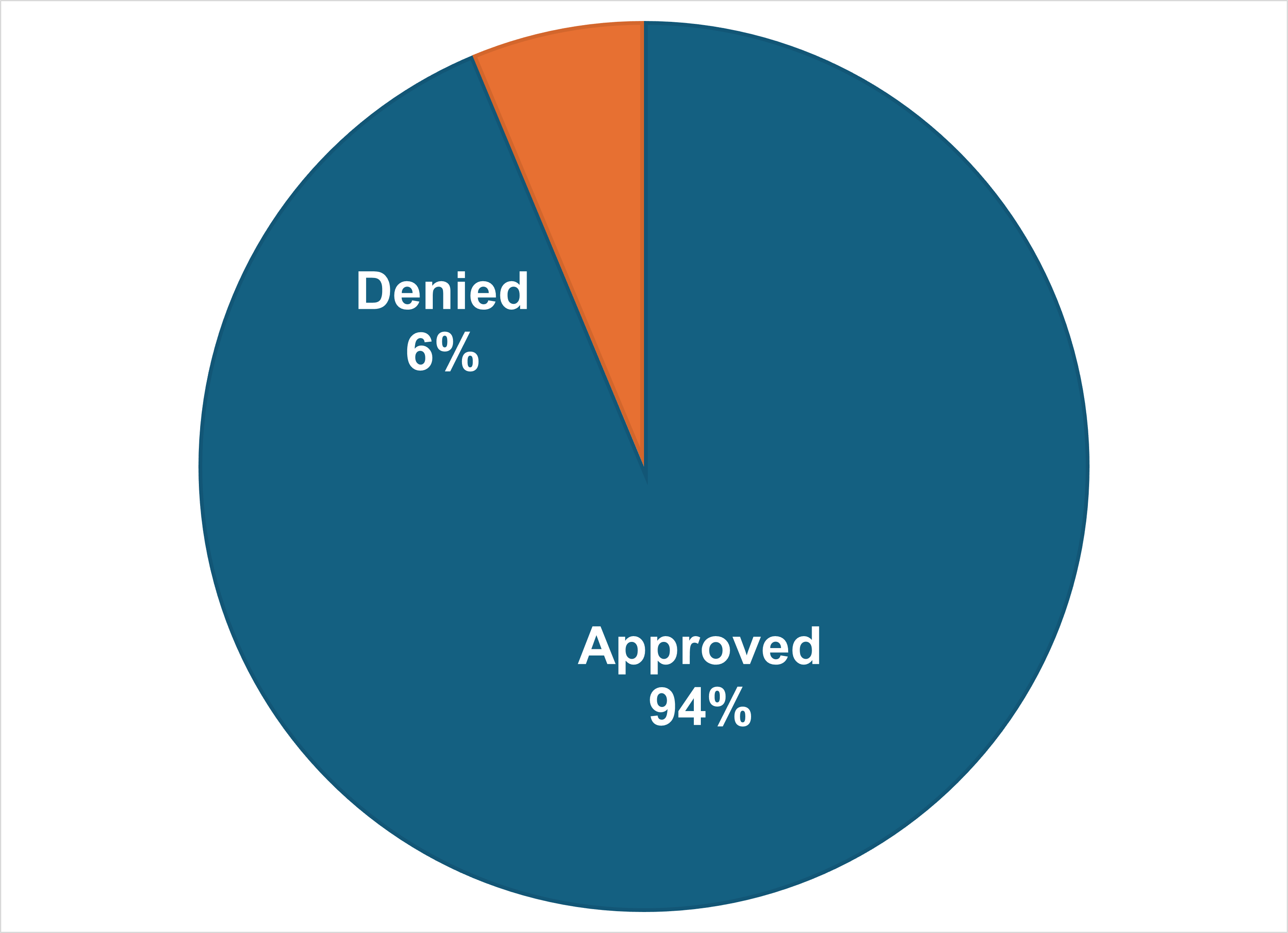
- Mean (average) time to make decisions: 1.3 days
- Median (middle) time to make decision: 1 day
Have questions about prior authorization?
CareAdvantage members
Call 1-866-880-0606 or 650-616-2174 Monday–Sunday 8:00 a.m. to 8:00 p.m.
TTY: 1-800-735-2929 or dial 7-1-1
Email: [email protected]
Medi-Cal and HealthWorx members and ACE Program participants
Call 1-800-750-4776 or 650-616-2133 Monday–Friday 8:00 a.m. to 6:00 p.m.
TTY: 1-800-735-2929 or dial 7-1-1
Email: [email protected]
